
Gut reaction: some of the tasty recipes that keep your gut healthy
‘Gut health’ has been trending on social media lately, and we couldn’t be happier. Your gastrointestinal tract is one of the most important (and complex) parts of your body. You probably know it performs the essential role of digesting and absorbing the nutrients you need to survive, but you might not be aware it is also responsible for regulating hormones AND it has a strong interaction with your immune system: 70–80 per cent of your immune cells live in your gut. Unfortunately, as with most popular topics, misinformation spreads faster than gastro in school, making it difficult to sort fact from fiction. So, what’s a person to do? Turn to our scientists, of course! Like microbiota bacteria on resistant starch, let us break down gut health for you.
Meals for microbiota

You’ve probably heard that a high-fibre diet plays an important role in helping to reduce the risk of colorectal cancers. Australia has one of the highest fibre intakes in the Western world, but bowel cancer has remained the nation’s second biggest cancer killer. So… what’s with that? Did scientists get it wrong? No, they’ve just learnt that when it comes to gut health, all fibre is not made equal. A particular type of fibre, resistant starch, is the big piece of the gut health puzzle that has been missing from most Western diets – something we hope to remedy.
Resistant starch is a special kind of starch that is indigestible, so it travels all the way through to your large intestine. While your body may not be able to digest resistant starch, it’s the perfect food for microbiomes. These special bacteria break down the resistant starch and release small carbohydrate molecules that other bacteria feast on. In turn, they release even tinier molecules called butyrate. Butyrate is absorbed by your large intestine which encourages blood flow, keeping your intestine healthy. Butyrate also helps your body detect damaged cells so they can be destroyed before turning into cancer.
So, is my gut healthy?
Fantastic farts
Do you fart or burp often? It may be embarrassing, but this could be a sign of good gut health. In a healthy gut, microbes are fermenting and as with any fermentation process, gas is produced and has to go somewhere. If it has trouble escaping, you can end up bloated and cramping which can be quite unpleasant, so don’t hold back! The average adult passes about 0.5 – 1.5 litres of ‘flatus’ a day, and even though gender has no bearing on the volume of gas produced, men tend to let rip around 12 times compared to women’s less frequent, but more voluminous, seven times per day. Of course, if you’re suddenly producing more gas than you usually do, or if they smell unbearable, this could mean you’ve got a gut issue worth talking to a health professional about.
The perfect poo
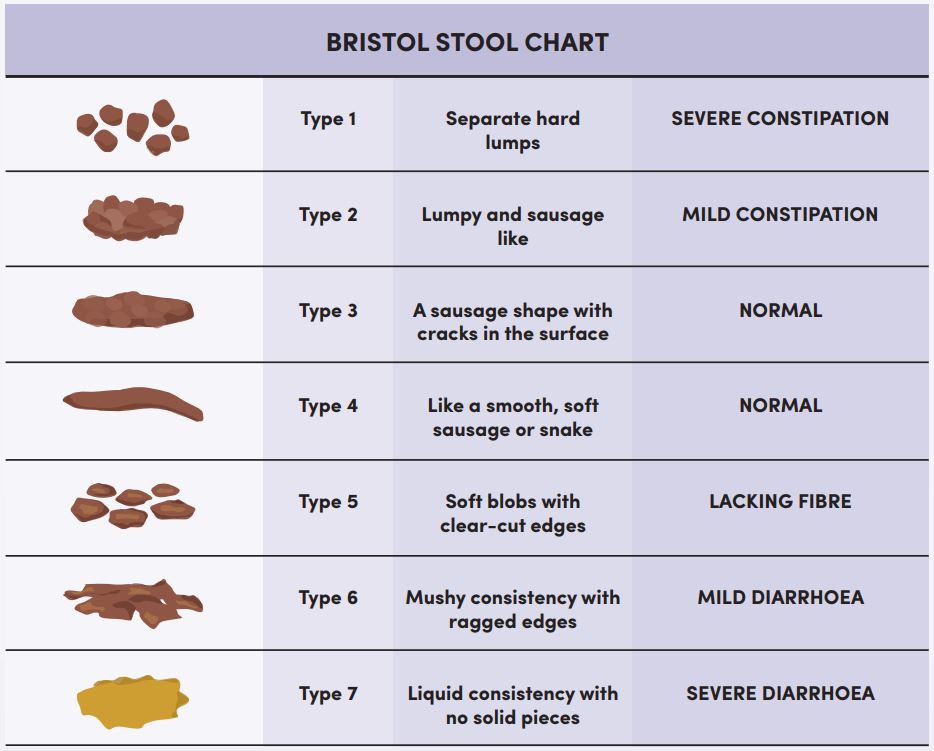
You may be surprised to hear that the frequency of your poo is actually less important than you might think: anywhere between three times a day and three times a week is within the normal range. Also surprisingly, your genetics have a lot to do with how often you poo, but frequency is also strongly influenced by our fibre intake, so no excuses! It’s worth mentioning that if you have a very slow ‘transit time’ (the time it takes for food to move through your gut) and your poo doesn’t weigh much you may be at greater risk of developing gut diseases and disorders, so yet another reason to keep up your fibre intake. The ‘perfect poo’ should be soft, light to deep brown, smooth and cylindrical. If it’s hard, lumpy or flattened, involves urgency, straining or lasting discomfort, things aren’t working quite right.
Unfortunately, the symptoms for many serious gut health problems are very similar to many harmless disorders so it can be tough to know when to see a doctor. Some signs that it’s time to visit the doc include; a sustained change in bowel movements; prolonged, severe or recurring pain; poo that is either black, greyish or has blood or mucus in it; unexplained weight loss; or difficulty swallowing. Importantly, don’t try and self-treat symptoms as you can make matters much worse.
Got a gut feeling?
So, you’re keen to improve your gut health, what next? Prepare yourself for mouth-watering recipes put together by our microbiota masters in The CSIRO Healthy Gut Diet, a book full of the latest research, gut health explainers and 85 tasty treats to help improve your gut health and resistant starch intake.


11th October 2018 at 10:06 am
All the pictured foods are the ones, that after years of eating them and suffering terrible IBS and diarrhoea, I have very recently cut out. I now do normal fragrant stool. My life has improved markedly since I deliberately cut out resistant starch. Resistant starch does indeed cause fermentation. The assumption here is that the fermentation is good. It may be fermentation of bad bacteria, not good.
I think the article’s advice is for people who actually have a poor diet that causes constipation. If you don’t, I suggest you do not follow this prescription. Eating fruit and veg gives you ample fibre. Excess will cause havoc with your biome.
11th October 2018 at 9:53 am
Not mentioned in the text, but hinted at in the picture, was the fact that cooling some foods after cooking increases their resistant starch. I found one paper titled “Effect of cooling of cooked white rice on resistant starch content and glycemic response” that measured a more than twofold increase in resistant starch when rice was cooked, cooled for 24 hours at 4°C and then reheated
11th October 2018 at 9:25 am
Why is it that cooked and cooled rice, potato and pasta has higher distant starch than when those carbs are uncooled?
11th October 2018 at 9:17 am
Thanks! The picture of foods high in resistant starch specifically says that some of the items are “cooked and cooled”. Does that mean that those foods are not as high in resistant start when eaten warm?
18th October 2018 at 3:49 pm
Hi Martin,
We asked the scientists involved and this was their response:
“Generally, the resistant starch content declines when foods are cooked but resistant starch can also be formed when the cooked food is cooled and stored for a period of time. For instance, potatoes that are cooked and then eaten contain mostly digestible starch and little resistant starch. However, when cooled, the structure of the starch gradually changes (there is a re-association or rearrangement of starch molecules) resulting in a slight rise in resistant starch content. This process is known as retrogradation.”
Cheers,
Eliza – social media team
11th October 2018 at 9:16 am
What is in the white bowl adjacent to the pasta???
11th October 2018 at 2:26 pm
Hi there, Charles – that’s brown rice. Thanks, Jesse, CSIRO, Social Media team.