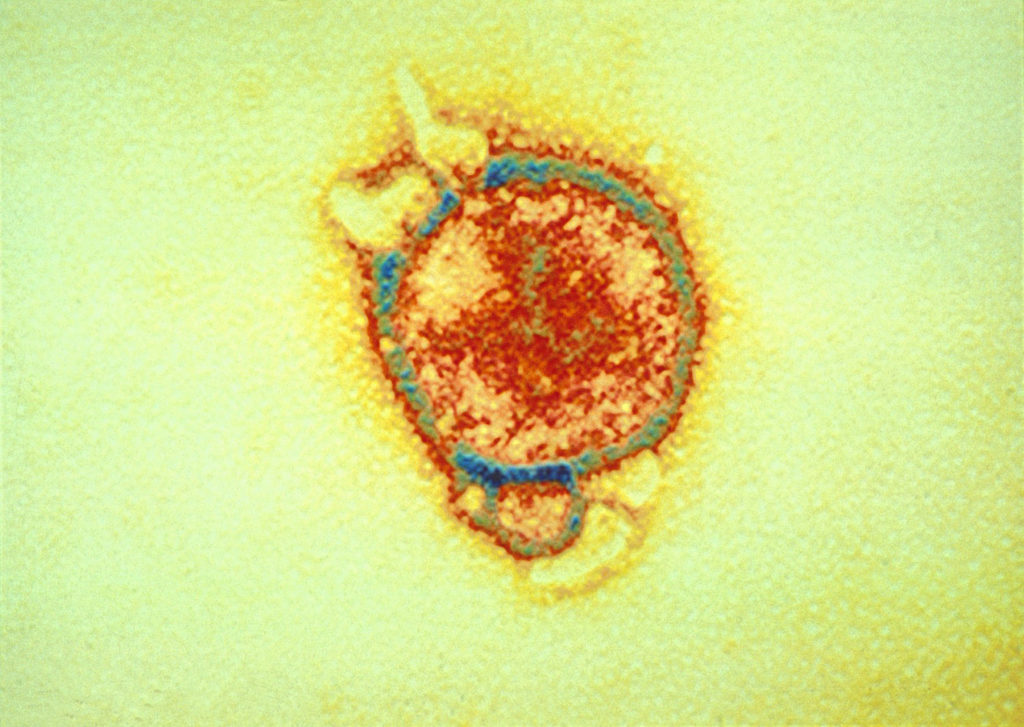
Electron micrograph of Hendra virus.
Last week Queensland’s Department of Heath announced they will soon begin testing a human antibody treatment against the deadly Hendra virus with the help of humans.
‘Hendra’ is a potentially fatal virus that can cause disease and death in horses and, occasionally, people. The virus is found in flying foxes, which are interestingly naturally immune to it.
The announcement of human trials is particularly exciting for us because of our intimate history with this virus and our involvement in the development of the monoclonal antibody in question – m102.4.
Hendra virus first came into the spotlight in 1994, when Queensland horse trainer Vic Rail, his stable hand and many of his horses, became ill to a mystery disease. Working with the then Queensland Department of Primary Industries (QDPI) our crack diagnostic team isolated and identified the virus, naming it Hendra after the Brisbane suburb where the outbreak occurred.
The Australian Veterinary Association recommends that all horses in Australia are vaccinated against the Hendra virus.
Sadly Vic and 14 of his horses succumbed to the virus, and since then several more outbreaks have occurred in horses in both Queensland and New South Wales. Of the seven human Hendra virus cases in Queensland, four people have sadly lost their lives.
Fast forward 19 years from the initial discovery and we have the development of the Equivac® HeV, the world’s first commercially available Hendra virus vaccine for horses – an achievement that was the culmination of a scientific and collaborative journey.
We have proven that this vaccine protects horses from a lethal exposure of the Hendra virus six months post vaccination, but what about protecting the health of people living and working around these beautiful animals?
The recent development of the ‘seek and destroy’ human monoclonal antibody known as m102.4 was truly a global effort. Our scientists were instrumental in the preliminary in vitro and in vivo (animal studies) work undertaken at the sophisticated high containment facilities at the Australian Animal Health Laboratory (AAHL) and provided critical expertise on the Hendra virus at the highest level of biosafety.
The laboratory-produced molecule works by attaching itself to the Hendra virus, preventing it from causing an infection.
The purpose of administering the monoclonal antibody is to treat Hendra virus infection in people and to improve the survival rate of those who have come in contact with infected horses. Although m102.4 has already been used on compassionate grounds to treat eleven people, ten of whom survived, no formal human safety trials have yet been undertaken. This is where the volunteers come in.
Australian Animal Health Laboratory (AAHL) has been actively involved and has worked closely with QDPI and Queensland Health in each recorded Hendra virus incident since it first emerged in 1994.
Queensland’s Department of Health is seeking local volunteers for phase 1 safety trials of m102.4 which will be run at the Q-Pharm clinics at QIMR Berghofer Medical Research Institute under the supervision of Princess Alexandra Hospital’s respected Hendra virus specialist Dr Geoffrey Playford. You can find out more about the trial here.
The m102.4 was developed by Dr. Chris Broder at the Uniformed Services University of the Health Sciences, Maryland USA. Queensland Health has further developed the antibody (with funding from Australian Institute for Bioengineering and Nanotechnology) by purifying and making safer for human use. Queensland Health has developed batches of m102.4 to ensure sufficient supply for compassionate use.



