By Emily Lehmann

Dr Edwards with mesh made by our warp knit machine in the background.
As many mums say, there is no better gift than to bring a child into the world.
What we wish most is that when the baby arrives, both mother and child are happy and healthy. However, between the pregnancy and delivery a myriad of complications can arise.
One common condition that affects almost one in four Australian women is pelvic organ prolapse.
It most often occurs as a result of childbirth when one or more organs descend from where they should be as a result of weakened ligaments, muscles and supporting tissue. The early stages can sometimes go unnoticed, but later symptoms include incontinence and sexual dysfunction.
Milder forms are treated through exercise and therapeutic medical devices (pessaries), while more severe cases require reconstructive surgery, where permanent mesh implants are added to support and aid tissue repair. In fact, it’s estimated that one in five Australian women will have surgery for the condition at some stage in their life.
Unfortunately, current mesh implants are known for causing complications.
So we’ve teamed up with researchers from Monash University to develop a new and improved mesh. It will have better mechanical properties, with the addition of stem cells to speed up tissue repair and treat the condition more effectively.
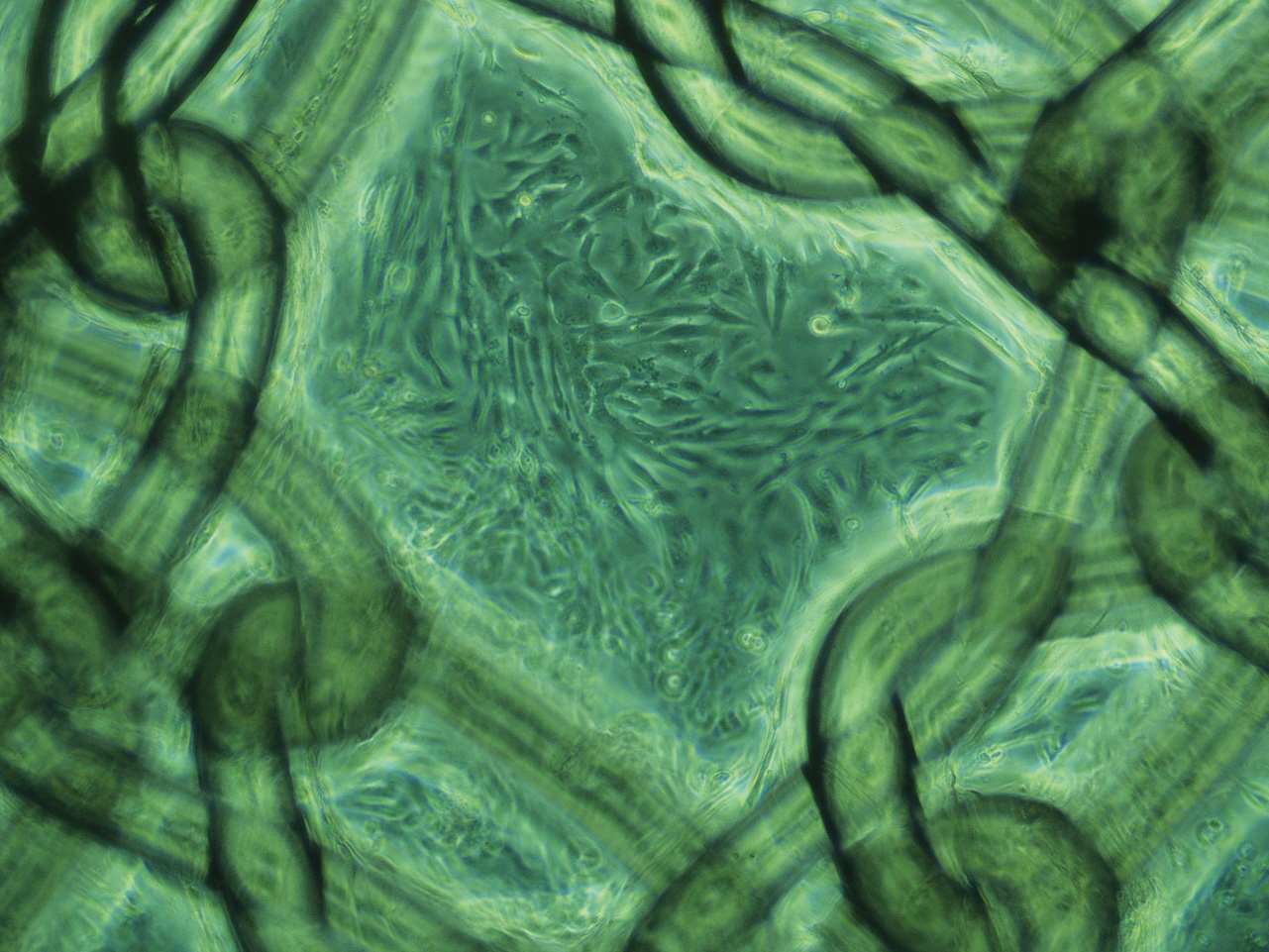
Tissue engineered mesh with seeded stem cells.
“Current mesh implants are problematic because they haven’t been designed for this purpose. They are rigid like a piece of cardboard when really they need to be flexible to move with the surrounding tissue,” says CSIRO textiles expert, Dr Sharon Edwards.
“This can cause women a range of issues including pain, discomfort, fibrosis and erosion, and in some cases further surgery is required.”
The team is investigating the use of a different polymer and warp knit pattern to fabricate a mesh that’s lightweight, elastic and porous.
“Our aim is to increase comfort, reduce the likelihood of complications and create better long-term health outcomes,” says Dr Edwards.
Dr Edwards explains how the mesh works in more detail:
Find out more about how CSIRO’s health research in our interactive web graphic.
Media: Emily Lehmann T: +61 3 9545 8746 M: +61 419 271 822


26th October 2014 at 11:02 pm
Hello, Is there any update as to when this mesh will be ready?
Will it be ready for next year? I am prepared to use it in a trial if possible.
Kind regards,
Michelle
24th July 2014 at 10:52 am
Hello, Is there any current updates about when the new mesh would be ready? I am prolonging surgery to wait for this safer alternative.
29th July 2014 at 3:17 pm
Hi Michelle,
The mesh is still under development as the researchers determine the ideal properties and best way to create it – so it will be some time before it is available. The best person to speak to about your options is your doctor.
Cheers,
Crystal
22nd June 2014 at 5:37 am
This is wonderful news …
16th June 2014 at 3:03 pm
I have just had prolapse repair WITHOUT mesh because of the complications caused through the use of polypropylene mesh. There is a chance that the prolapse will re-occur so I will be watching and hoping that a new improved safer mesh will be there if I need it. Best wishes to all, Jenny Sykes.
10th May 2014 at 4:40 pm
Hi there, when will the new and improved mesh be available?
15th May 2014 at 10:12 am
Hi Liz,
At this stage the mesh is still under development. Once our researchers have determined the ideal properties and the best way to create it, we hope to make it available to the public. We’ll keep you posted.
Cheers,
Steph