Our scientists at the Australia e-Health Research Centre have partnered with the Hollywood Private Hospital in Perth to conduct the world’s first large scale ocular biomarker study for mental health disorders.
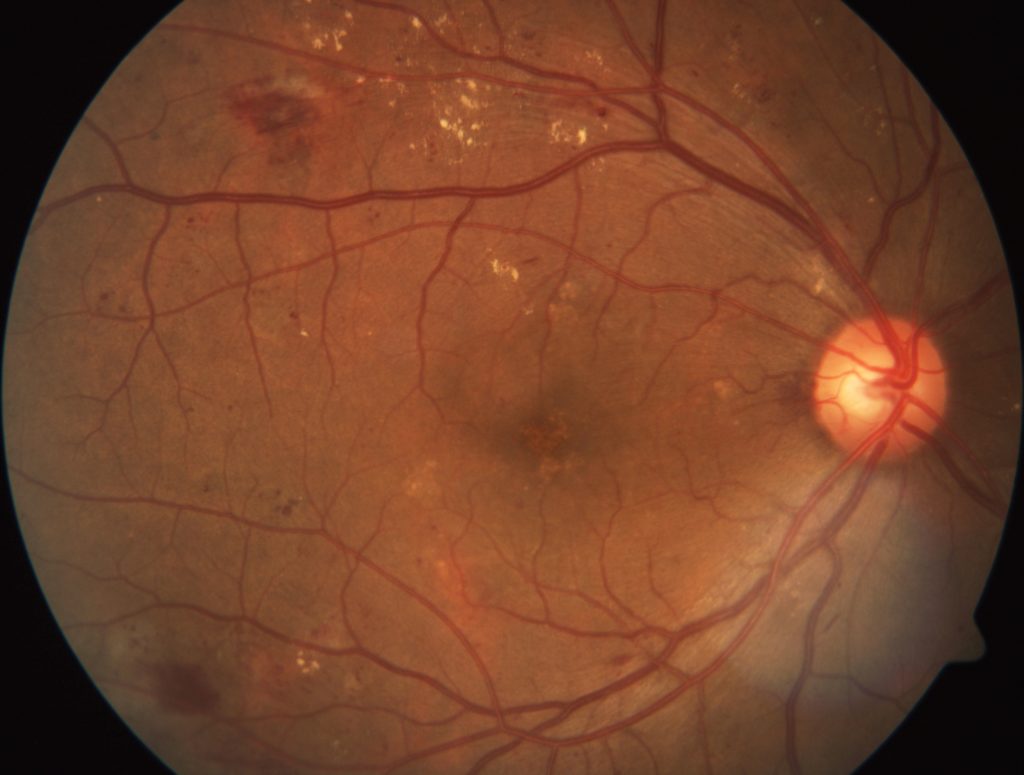
Retinal images like this one here may hold to the key to detecting mental health disorders.
The eyes have often been quoted as being the ‘windows into the soul’, but what if they are actually windows into our brain?
Some neurological conditions, such as schizophrenia, are accompanied by physiological changes in the eye. In fact nearly 60 percent of adult schizophrenia patients experience some kind of vision distortion.
Do these changes, or different ones, occur in other brain disorders? And if so, could detection of tiny changes in our eyes be used to predict, diagnose and monitor conditions such as post-traumatic stress, anxiety, eating disorders, major depression and alcohol dependence?
To answer these questions our scientists at the Australia e-Health Research Centre have partnered with the Hollywood Private Hospital in Perth to conduct the world’s first large scale ocular biomarker study for mental health disorders.
This collaborative research project will investigate whether monitoring changes in the retina can allow specialists to more effectively detect and diagnose brain disorders.
Current methods of diagnosis for these mental health disorders are complex and subjective, making diagnosis difficult and misdiagnosis frequent – which means patients aren’t always getting the best treatment for their illness.
The trial will look deeply into the eyes of 200 patients using retinal photography, optical coherence tomography and pupillometry to try to determine if eye biomarkers are specific to different disorders, and if they can be used for early detection and diagnosis.
A simple detection and diagnosis system for mental health illness … that’s our vision.
Find out how we’re using technology to save the sight of rural and remote Australians.


11th September 2016 at 7:23 am
Non-invasive.
8th September 2016 at 7:20 pm
Many mentalhealth disorders have a HPA axis dysfuntion which can be detected in simple urine and blood tests. For instance PTSD in Combat veterans presents with reduced 24 hour urine cortisol and supressed cortisol production in overnight stress…… so my insurance company wants me to have MDD instead of PTSD because it is cheaper for them. My tests confirm PTSD or Possibly PTSD+ MDD but not MDD alone so they kind of have made things woorse for themselves – this knowledge has been around for at least 14 years and researched a lot – but it is in not used for diagnosis in the manual – Insurance love the ambiguity of mental health diagnosis and always try for a cheaper differential diagnosis – regardless of the impact that has on a persons wellbeing. So if you are successful please lobby for the biological signs to be included in the diagnostic manuals
8th September 2016 at 7:30 pm
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4518698/ HPA disfunction discussed here
8th September 2016 at 2:15 pm
Sounds like CSIRO is following the Dunedin Study and claiming it as their own.