We are testing two vaccine candidates at our Australian Centre for Disease Preparedness (formerly Australian Animal Health Laboratory or AAHL) in Geelong, Victoria.
Updated 24 April 2020
After months of research, we have a major update on our COVID-19 work. We have started pre-clinical trials for two vaccine candidates. This is happening at our Australian Centre for Disease Preparedness (ACDP) in Geelong, Victoria.
The work — in which we play a critical role — involves deep collaboration within Australia and overseas and forms part of a global rapid response to this pandemic.
Pre-clinical trials to get the vaccine faster
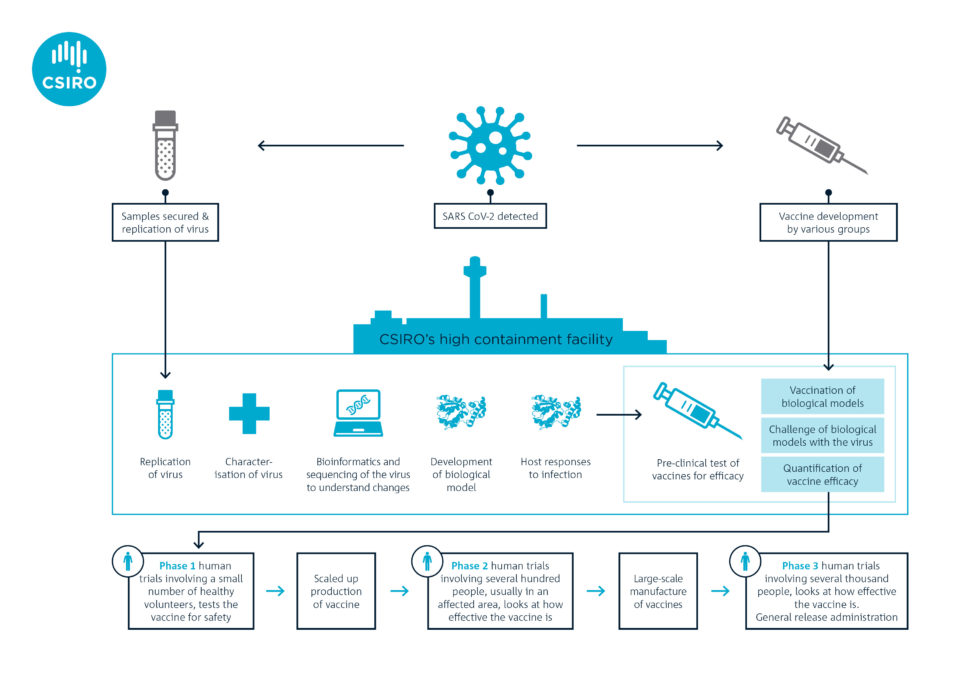
Vaccines generally take 10-15 years to develop and test. But researchers like us are hoping to streamline this process. We’re working as part of a global alliance with the Coalition for Epidemic Preparedness Innovations (CEPI). The goal is to speed up traditional vaccine development and testing and have at least one vaccine ready within 10-15 months.
CEPI asked us in January to start getting a better understanding of COVID-19 while the outbreak was in its early stages. We were the first research organisation outside of China to generate enough stocks of the virus (using the VIC01 strain isolated by the Doherty Institute) for preclinical research.
In February, we became the first team in the world to show that ferrets are susceptible to this novel coronavirus. We established the ferret model in record time and were tasked by CEPI in March to start the world’s first multi-vaccine efficacy study in animals.
In consultation with the World Health Organization (WHO), CEPI selected two candidates based on readiness for testing. The vaccine candidates come from Inovio Pharmaceuticals in the US and the University of Oxford. They’re the second and third vaccines in the world to undergo pre-clinical trials. The former is a DNA vaccine, a novel approach because there are currently no licenced DNA vaccines for humans. The latter is what’s called a vectored vaccine (an established technology).
Pre-clinical trials are underway at our high containment facility, the Australian Centre for Disease Preparedness (ACDP)
Phase 1 clinical trials
Both candidates are now entering Phase 1 clinical trials in healthy humans to see if they are safe. However, before seeking approval for Phase 2 and Phase 3 clinical trials, vaccine developers need efficacy data from pre-clinical studies. This is where organisations such as ours play a major role.
The two vaccine candidates are undergoing pre-clinical trials in our laboratory. Ferrets will be vaccinated and monitored for four weeks so it develops immunity. The ferrets will then be given a dose of the virus to measure the success of the two vaccine candidates. Such studies are planned very carefully with significant oversight of animal ethics and welfare considerations.
We’re not directly involved in developing vaccine candidates for COVID-19. But our preclinical trials are critical in helping to refine possible vaccination strategies. For example, we will test less invasive routes of vaccination (e.g. via the nose) and a two-shot regimen. The findings from our studies can have a huge impact on clinical delivery.
What else is happening at CSIRO?
We studied SARS-CoV-2’s genome sequence and confirmed the virus is changing into distinct clusters. We’re now looking at how this may impact the development and evaluation of COVID-19 vaccines, therapeutics and diagnostic tests.
In partnership with The University of Queensland, our researchers have successfully demonstrated the presence of SARS-Cov-2 in Australian untreated wastewater. This is the first step in developing an early warning surveillance system to track COVID-19 prevalence in the community.
We’re also working with the Australian Government and Victorian manufacturers to build local capability and supply of materials. This will rapidly address the demand for medical materials. And with one vaccine (developed by the University of Queensland), we are helping to scale-up production.


17th April 2020 at 10:15 am
Is there a way to “super-charge” the vaccine or perhaps the immune system? Has any work been done on the use of targeted radiation on covid19 cellular structures?
23rd April 2020 at 4:09 pm
Hi Alan, thanks for your message.
It’s not something our researchers can answer at this stage. Any key developments we will share via our social media channels.
Thanks,
Kashmi
Team CSIRO.
16th April 2020 at 9:03 pm
What impact would skipping a double blind study have upon the time line of fielding a vaccine? I can see that there might be ethical issues in performing a double blind study where it would be conducted during the human trial phase. What would the replacement be for not doing a double blind study if it came down to it in determining the potency and safety of the vaccine? Would a single blind study be sufficient enough to determine if a vaccine is effective?
16th April 2020 at 5:57 pm
Keep up the good work folks. I see that we are looking at the use of HIV/Legionaires and Maleria medication. Professor Didier RAOULT of France has already had good success with using both hydroxychloroquine and azithromycin on some 160 patients. Not sure if our friends in Qld are familiar with his work. But thank you all for the great job that you are doing. ?
16th April 2020 at 2:53 pm
CSIRO you are so critically important! Perhaps the present Government might recognise this now and lament their disastrous funding cuts to you in the recent past. Thankyou for all the fantastic work you all do.
16th April 2020 at 2:12 pm
What happened to the University of Queensland research ?
23rd April 2020 at 4:09 pm
Hi Ian, thanks for your question.
This research is still underway. Any key developments will be shared via our or UQ’s social media channels.
Kind regards,
Kashmi
Team CSIRO